Armenta Washington, MS, senior research coordinator (pictured above), has made it her mission to change that. Soon after joining the Abramson Cancer Center in March 2020, Washington, in collaboration with Associate Director of Diversity and Outreach, Carmen Guerra, MD, MSCE, FACP, started developing the curriculum for the Abramson Cancer Center’s inaugural Clinical Trials Ambassador Program. The goal of the program is to educate lay volunteers on cancer and cancer research — and train them to be ambassadors for clinical trials in their communities.
After completing the 10-week program, the first cohort of 19 ambassadors graduated on Oct. 14, 2021. The graduates represent a diverse group of cancer patients, survivors and caregivers representing a wide variety of education levels and socioeconomic backgrounds. Washington, along with colleagues from Abramson Cancer Center and the National Cancer Institute (NCI) led the eight weekly two-hour virtual sessions, during which participants learned:
- What cancer is and how it develops
- Why research is important
- Why it is necessary to have diversity in clinical trials
- What type of research is conducted at Abramson Cancer Center
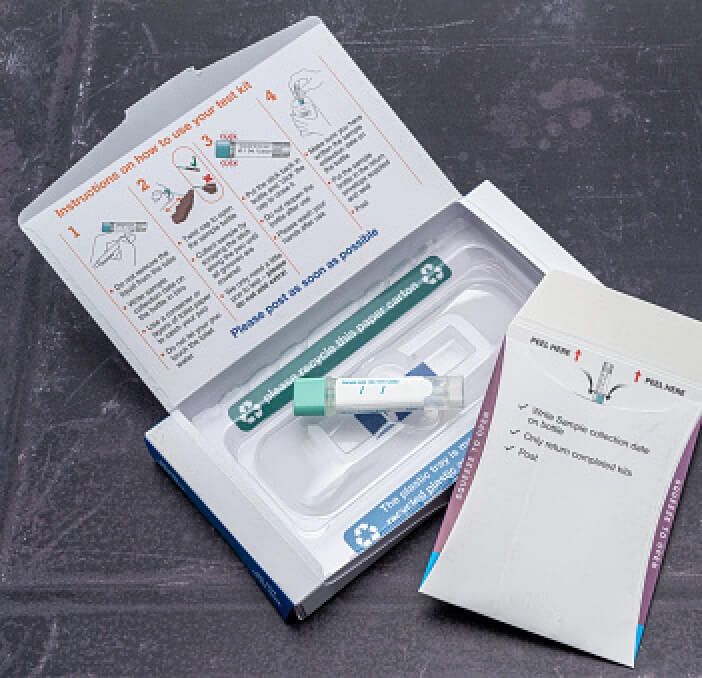
- What biospecimen research is and how biobanking works
- About clinical trial patient protections the Abramson Cancer Center has in place
The program also created clinical trial brochures with messaging tailored specifically to Black people with cancer. A significant portion was dedicated to training participants on how to talk to people in their communities about cancer research, using the brochure to supplement the conversation.
"The expectation is that they will, in their natural networks when the conversation comes up, be prepared to engage and talk about what they’ve learned about clinical trials and encourage patients to have a conversation with their physician," Washington says.
Washington and Dr. Guerra are also working on other opportunities for the ambassadors to make a difference, such as inviting them to mentor cancer patients, speaking on panel discussions or providing a patient perspective for grant proposals.